#18,028
This afternoon the
WHO, FAO and
WOAH have published a joint
8-page preliminary assessment of HPAI H5N1 viruses which have recently spilled over into cattle in the United States, along with many other mammals around the globe.
Today's joint assessment pegs the overall public health risk posed by A(H5N1) to be low, but is low-to-moderate for those with exposure to infected birds, animals, or contaminated environments.
First the overview, followed by some excerpts from the full document. Follow the link to read it in its entirety.
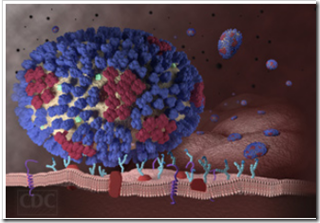
During 2020, highly pathogenic avian influenza (HPAI) A(H5N1) clade 2.3.4.4b viruses arose from previously circulating influenza A(H5Nx) viruses and spread predominantly via migratory birds to many parts of Africa, Asia and Europe. The epizootic has led to unprecedented numbers of deaths in wild birds and caused outbreaks in domestic poultry. In late 2021, these viruses crossed to North America and subsequently South America in October 2022.
Additionally, globally, there have been increased detections of A(H5N1) viruses in non-avian species including wild and domestic (including companion and farmed) terrestrial and marine mammals and, more recently in goats and dairy cattle in the United States of America.
Since the beginning of 2021, 28 detections of A(H5N1) in humans have been reported to WHO, including a case who had exposure to dairy cattle presumed to be infected with A(H5N1) virus. Of these human cases, where the haemagglutinin (HA) H5 clade is known, 13 have been caused by clade 2.3.4.4b viruses. This joint FAO/WHO/WOAH risk assessment focuses on A(H5N1) viruses characterized since 2021 and assesses the public health risk as well as the risk of the virus spread among animals.
23 April 2024
(Excerpts)
During 2020, highly pathogenic avian influenza (HPAI) A(H5N1) clade 2.3.4.4b viruses arose from
previously circulating influenza A(H5Nx) viruses and spread predominantly via migratory birds to
many parts of Africa, Asia and Europe. The epizootic has led to unprecedented numbers of deaths in
wild birds and caused outbreaks in domestic poultry.
In late 2021, these viruses crossed to North
America and subsequently South America in October 2022. Additionally, globally, there have been
increased detections of A(H5N1) viruses in non-avian species including wild and domestic (including
companion and farmed) terrestrial and marine mammals and, more recently in goats and dairy cattle
in the United States of America. The majority, with some regional exceptions, of the HPAI A(H5N1)
viruses characterized genetically since 2020 belong to the 2.3.4.4b clade.
Since the beginning of
2021, 28 detections of A(H5N1) in humans have been reported to WHO, including a case who had
exposure to dairy cattle presumed to be infected with A(H5N1) virus. Of these human cases, where
the haemagglutinin (HA) H5 clade is known, 13 have been caused by clade 2.3.4.4b viruses.
This joint
FAO/WHO/WOAH risk assessment focuses on A(H5N1) viruses characterized since 2021 and assesses
the public health risk as well as the risk of the virus spread among animals.
Infections in animals
Avian influenza A(H5N1) viruses, especially those of clade 2.3.4.4b, continue to diversify genetically
and spread geographically. Since 2022, a broader range of wild bird species has been infected
globally which has had deleterious ecological consequences and caused mass die-offs in some
species. The situation with wild mammals is also worrying, with some species suffering significant
mortality events.
Additionally, ongoing circulation in wild and migratory birds and poultry has led to multiple separate
incursions into wild carnivorous and scavenging mammals, domestic cats and dogs, and aquatic
mammals in a number of countries.
Spillover of clade 2.3.4.4b viruses from birds to mammals in the
Americas and Europe have often resulted in severe infections with neurological signs in some
mammals.1
In 2024, A(H5N1) viruses have been detected in neonatal goats on a single premises
shared with poultry, and in dairy cattle in the USA.
These circumstances have led to increased opportunities for viral reassortment generating new
genotypes with varied clinical signs.
(SNIP)
Assessment of current risk to humans posed by influenza A(H5N1) viruses
1. What is the global public health risk of additional human cases of infection with avian influenza
A(H5N1) viruses?
Despite the high number of A(H5N1) clade 2.3.4.4b outbreaks and detections in animals, and
human exposures to the virus at the human-animal-environment interface, relatively few human
infections have been reported to date.
Of the 28 human cases of A(H5N1) detections reported since the beginning of 2021, all were
sporadic infections in people exposed to A(H5N1) viruses through direct or indirect contact with
infected birds, infected mammals or contaminated environments, such as live poultry markets or
other premises with infected animals. Among these cases, there has been no reported human-to-human transmission.
While the viruses continue to be detected in animals and related environments, including milk,
further sporadic human cases among exposed individuals are expected. Active case finding
around reported human cases has been ongoing, and should continue, to determine if there is
any human-to-human transmission.
Individuals with activities that involve exposure to infected animals and/or contaminated
environments are at higher risk and should take necessary precautions to prevent infection.18
At the present time, based on available information, WHO assesses the overall public health risk
posed by A(H5N1) to be low, and for those with exposure to infected birds or animals or
contaminated environments, the risk of infection is considered low-to-moderate. This risk
requires close monitoring and WHO and partners will continue to regularly assess and publish
public health risk assessments for avian influenza.
What is the likelihood of cattle-to-human transmission of influenza A(H5N1) viruses?
Human cases have followed exposure to avian influenza-infected mammals for other influenza A
subtypes, including A(H7N2)19 and A(H7N7)20, but only in a few instances. To date, there has been
one reported case of infection with an influenza A(H5N1) virus in the USA in a person who worked at
a dairy farm where cattle were presumed to be infected with A(H5N1) viruses. This case presented
with conjunctivitis as the only symptom and has since recovered.
Infected lactating cattle have been reported to have high viral loads in their milk and thus could be a
source of exposure to persons in close contact with them.21 The potential role of consumption and
handling of milk and milk products in transmission, and the role of pasteurization in mitigating the
potential risk, is currently being investigated.
As long as people are in contact with infected cattle without appropriate personal protective
equipment, there is a risk for human infections. The risk can be mitigated by measures to reduce
exposure to the virus, such as the use of recommended personal protective equipment, appropriate
personal hygiene and other risk-based biosecurity measures.
3. What is the likelihood of human-to-human transmission of avian influenza A(H5N1) viruses?
There has been no reported human-to-human transmission of A(H5N1) viruses since 2007, although
there may be gaps in investigations. Prior to 2007, small clusters of A(H5) virus infections in humans
were reported, including some involving health care workers, where limited human-to-human
transmission could not be excluded; however, sustained human-to-human transmission was not
reported.22
The A(H5N1) viruses detected in mammals, including in human cases, largely retain genomic and
biological characteristics of avian influenza viruses and remain well-adapted to spread among birds.
Except for in-host obtained amino acid mutations in polymerase proteins, there is still limited
evidence for adaptation to mammals and humans even when transmission in mammals has been
suspected.23 No changes in receptor binding tropism have been observed that would increase
binding to receptors in the human upper respiratory tract which would increase transmission to and among people. Therefore, human-to-human transmission of the currently circulating A(H5N1)
viruses is considered unlikely without further genetic changes in the virus.
WHO, together with the Food and Agriculture Organization of the United Nations (FAO) and the
World Organisation for Animal Health (WOAH), continues to monitor these viruses and will re-assess
the risk associated with the currently spreading A(H5N1) viruses as more information becomes
available.
Further antigenic characterization of A(H5N1) viruses, including in relation to the existing CVVs, and
development of specific reagents are being prioritized at the WHO Collaborating Centres and
Essential Regulatory Laboratories of GISRS in collaboration with animal health and veterinary sector
colleagues.
(Continue . . . )