Photo Credit- CDC
# 8655
With the spring surge in MERS cases in the Middle East, and a (thus far) small number of exported cases to countries like Greece, Malaysia, The Netherlands, and the United States, we’ve seen a lot of talk (pro and con) on the pandemic potential of the emerging MERS coronavirus.
It’s an understandable debate, as a pandemic would have a huge global impact - and if one were in the wings -now is the time we should be preparing for it.
Although we’ve seen some impressively large clusters in healthcare settings, so far, the illness hasn’t spawned large outbreaks in the community, and its spread outside of the Arabian peninsula has been anemic. So far, the consensus appears to be that the MERS coronavirus is not yet sufficiently transmissible enough to spark a pandemic.
Good news. With the caveat being that viruses have a nasty habit of changing over time.
This disease’s future isn’t a binary one, however; a `pandemic or nothing’ proposition. Even in its present incarnation, it has the potential to be a long-term, high-impact problem.
Already, with just two introductions into the United States, we’ve seen its expensive and disruptive effects; hundreds of people potentially exposed, scores of healthcare workers furloughed to home isolation, extensive contact tracing & testing programs initiated, and scores of lives and jobs interrupted.
And while only impacting two healthcare facilities directly, the ripple effects – implementing better screening, testing, and heightened infection control in anticipation of future cases – extend to all medical facilities.
The irony is, that as long as a pathogen has unrealized `pandemic potential’, public health attempts to contain it in some ways are more extensive and disruptive than efforts to deal with it after it becomes a pandemic.
The arduous process of contact tracing and testing of potentially exposed airline passengers makes sense as long as the virus remains rare, but quickly becomes moot once a virus become pervasive in the community. Similarly, the public health value of stringent isolation and quarantine policies diminish as a pandemic progresses.
While better than dealing with a pandemic, fighting a `cold war’ against an emerging infectious disease threat can be protracted, expensive, and exhausting proposition – much like the battle that has been waged these past few years against emerging antibiotic resistant organisms like NDM-1 and CRE (see MMWR Vital Signs: Carbapenem-Resistant Enterobacteriaceae (CRE)).
The spread of HAIs (Hospital Acquired Infections) has cost us hundreds of thousands of lives and billions of dollars over the past decade, and despite elaborate measures taken to prevent them, the `bugs’ seem to be winning.
Even with limited `droplet or airborne’ transmissibility, MERS-CoV adds to the complexity of infection control in medical settings, meaning that even a handful of imported cases each month have the potential to severely impact healthcare facilities, and many lives, across the nation.
It doesn’t require a Stephen King-styled pandemic to turn MERS into a major problem. A small but steady influx of MERS cases could do that as well – particularly when stacked on top of the growing list of other emerging (although not necessarily pandemic) disease threats.
A partial list of ongoing or emerging global health threats we’ve discussed includes:
- The importation of West Nile Virus to North America in 1999 (see WNV: The Economic Costs Of An Invasive Arbovirus)
- The more recent arrival of Dengue Fever in Florida and Texas (see MMWR: Dengue Fever In Key West)
- Last fall’s Chikungunya outbreak in the Caribbean which now threatens North America (see ECDC: Caribbean Chikungunya Update)
- And the growing threat from antibiotic resistant bacteria (see NDM-1: A Matter Of Import)
To this short list you can add the continual spread of H7N9 and H5N1 avian flu viruses (see The Expanding Array Of Novel Flu Strains) in Asia and the Middle East, Polio in the Middle East and Africa, contaminated food or drugs, XDR-TB, and of course the one(s) we don’t even know about yet . . . Virus X.
All of which makes the recent cuts in public health spending all the more egregious, dangerous, and foolhardy.
A recent report from TFAH (Trust for America’s Health) finds a steady decline in the resources available to public health across the nation.
Investing in America’s Health: A State-by-state Look at Public Health Funding & Key Health Facts
May 2014
Trust for America's Health (TFAH) and the Robert Wood Johnson Foundation (RWJF) released Investing in America's Health: A State-by-State Look at Public Health Funding and Key Health Facts. This is the ninth time the report has been released.
In Investing, TFAH and RWJF examine public health funding and key health facts for each state, finding:
- Wide Variation in Health Statistics by State: There are major differences in disease rates and other health factors in states around the country. For instance, only 7.0 percent of adults in Alaska have diabetes compared to 13.0 percent in West Virginia, and 28.3 percent of adults in Kentucky are current smokers while only 10.6 percent report smoking in Utah.
- Cuts in State and Local Funding: At the state and local levels, public health budgets have been cut at drastic rates in recent years. According to a TFAH analysis, 33 states and Washington, D.C. decreased their public health budgets from FY 2011-12 to FY 2012-13. Budgets in 20 states decreased for two or more years in a row, and budgets in 16 states decreased for three or more years in a row.
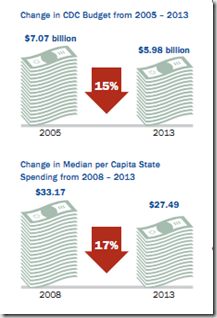
- In FY 2012-13, the median state funding for public health was $27.49 per person, ranging from a high of $144.99 in Hawaii to a low of $5.86 in Missouri. From FY 2008 to FY 2013, the median per capita state spending decreased from $33.71 to $27.49. This represents a cut of more than $1.3 billion (adjusted for inflation).
- Flat Federal Funding: Federal funding for public health has remained at a relatively flat level for years. The budget for CDC has decreased from a high of $7.07 billion in 2005 to $5.98 billion in FY 2013 (adjusted for inflation). Spending through CDC averaged to only $18.92 per person in FY 2013. And the amount of federal funding spent to prevent disease and improve health in communities ranged significantly from state to state, with a per capita low of $13.67 in Indiana to a high of $46.48 in Alaska.
Overall, the report concludes that the nation must shore up core ongoing funds for public health. In addition, the report recommends ensuring the Prevention and Public Health Fund is used to build upon and expand— not supplant – existing efforts.
Even as the number of global disease threats continue to rise, we seem blindly intent on gutting our only line of defense – our state, local, and Federal public health systems. In this climate of budget cutbacks, when combined with an ever growing list of other public health challenges, even dealing with a lighter shade of MERS may prove a serious challenge.
The old adage is true, `When public health works, nothing happens’.
The one thing we really, really don’t want to ever see in this country is what would happen if public health no longer worked.